- Surgical Treatment of Thymoma
Complete surgical resection is the gold standard in the treatment of thymoma. The development of minimally invasive techniques represents nowadays a valuable alternative to an open approach via median sternotomy. Several studies have been showing that video or robotic assisted approaches are comparable to open surgery in terms of oncological outcomes with lower morbidity rates, shorter length of stay and less pain.
Introduction
Thymomas are rare neoplasms arising from the epithelial component of the thymus in the anterior mediastinum. From a clinical and pathological point of view, a thymoma can have a wide features spectrum ranging from well differentiated and encapsulated masses up to undifferentiated tumours with an aggressive course. They usually affect patients in the fourth to sixth decade of life accounting for 0.2–1.6% of all malignant tumours (1).
Diagnostic
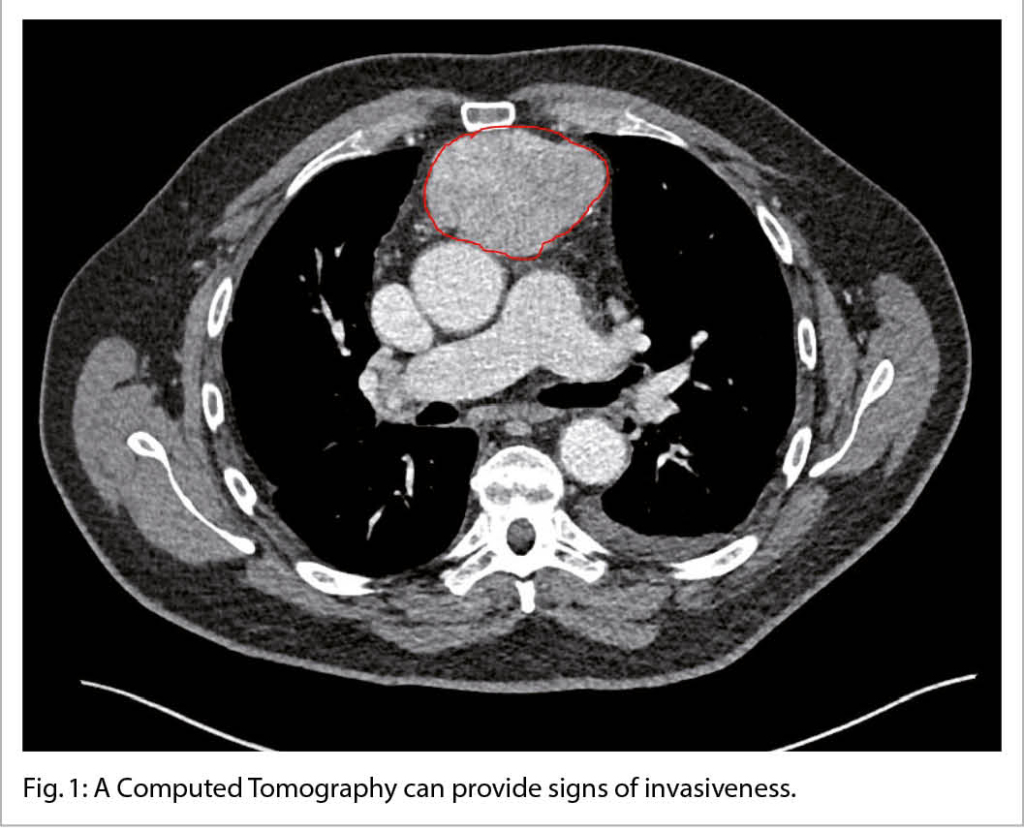
Roughly 30% of thymoma patients have no symptoms and the diagnosis is made incidentally based on radiological findings (2). Most of thymomas are visible on chest radiography as an ovoid mediastinal mass abutting unilaterally (very rare even bilaterally) and, on the lateral view, as a mass located in the retrosternal compartment. A Computed Tomography (CT) is considered the gold standard not only because is highly evocative of the diagnosis (fig. 1) but can also provide, especially when performed with intravenous contrast, signs of invasiveness (irregularity, unclear margins, an incomplete capsule, pleural or pericardial effusion, invasion of surrounding structures).
Fluorodeoxyglucose (FDG) positron emission tomography (PET) plays a controversial role in the diagnostic workup of thymic tumours (4). The presence of a FDG mass in the mediastinum is unspecific and can be referred to several conditions like infection, thymic hyperplasia, fibrosing mediastinitis or tumours other than thymoma (e.g., lymphoma or malignant germ cell tumours). Some authors advocate the use of PET/CT in the diagnostic pathway in order to differentiate low-grade from high-grade thymic tumours, but several studies reported these findings as controversial. In several centers, PET/CT plays a role only in the detection of distant metastasis especially when the primary tumour shows an aggressive behaviour.
When the patients are symptomatic, they usually report unspecific symptoms such as chest discomfort/pain, cough and dyspnoea. Sometimes, especially when thymoma shows an aggressive behaviour symptoms deriving from mass effect in the mediastinum are present (superior vena cava syndrome, phrenic nerve palsy, stridor, dysphagia).
Systemic symptoms are predominant when thymomas are associated with autoimmune disorders such as myasthenia gravis, pure red cell aplasia and hypogammaglobulinemia.
Surgical management
Surgical resection is usually the gold standard for the treatment of patients with thymoma. Three different approaches are described in the literature: transsternal via sternotomy, transcervical and minimally invasive via Video-Assisted Thoracoscopic Surgery (VATS) or Robotic Assisted Thoracoscopic Surgery (RATS).
A median sternotomy has been historically the gold standard due to the excellent exposure of the mediastinum. A transcervical approach has the advantages that the wound is small, there is no need for a thoracic drain post-operative, the patients have less pain and therefore their length of stay is shorter (5). If the patient is unable to extend the neck, this approach is usually not recommended.
Several authors are skeptical about the possibility to achieve a complete resection with this approach but several trials showed outcomes comparable with other approaches (6).
Over recent years, VATS or RATS thymectomies are becoming increasingly used in several centers through a multi- or uniportal approach. The advantages of a minimally invasive approach have been published in several papers, specifically it is worth highlighting low postoperative morbidity and mortality, shorter length of stay along with a relative low (0% to 7%) conversion rate to open surgery (7). In addition, several comparison studies showed that the oncological outcomes after a minimally invasive thymectomy are comparable to those after a thymectomy performed via median sternotomy (8).
Recently, a subxiphoid uniportal approach has been reported in several papers (9). Compared to the intercostal VATS or RATS approach, a subxiphoid uniportal VATS thymectomy represents a less invasive variant providing an excellent view of the bilateral pleural cavities with the advantage to save the intercostal space and, thus, causing less pain in the post-operative period.
Copyright bei Aerzteverlag medinfo AG
Leitender Arzt
Luzerner Kantonsspital
Klinik für Thoraxchirurgie
Haus 31
Spitalstrasse
6000 Luzern 16
Chefarzt
Luzerner Kantonsspital
Klinik für Thoraxchirurgie
Haus 31
Spitalstrasse
6000 Luzern 16
Die Autoren haben keine Interessenkonflikte im Zusammenhang mit diesem Artikel deklariert.
◆ The treatment’s keystone of thymoma is the patient’s selection
performed with a multidisciplinary approach.
◆ For patients considered candidates for surgery, radicality is the most important prognostic factor.
◆ Even if historically an open resection was considered the gold
standard, nowadays a minimal invasive approach can be considered safe and feasible when performed by experienced surgeons.
J Thorac Dis 2020;12:7613-8.
2. Minervini F, Boschetti L, Gregor M, Provencio M, Calvo V, Kestenholz PB, Lampridis S, Patrini D, Bertoglio P, Azenha LF, Sergi CM, Kocher GJ. Thymic tumours: a single center surgical experience and literature review on the current diagnosis and management of thymic malignancies. Gland Surg. 2021 Nov;10(11):3128-3140. doi: 10.21037/gs-21-517. PMID: 34926228; PMCID: PMC8637068.
3. Benveniste MF, Korst RJ, Rajan A, Detterbeck FC, Marom EM, International
Thymic Malignancy Interest G. A Practical Guide From the International
Thymic Malignancy Interest Group (ITMIG) Regarding the Radiographic Assessment of Treatment Response of Thymic Epithelial Tumors Using Modified RECIST Criteria. J Thorac Oncol (2014) 9(9 Suppl 2):S119–24. doi: 10.1097/JTO.0000000000000296
4. Viti A, Terzi A, Bianchi A, Bertolaccini L. Is a positron emission tomography-
computed tomography scan useful in the staging of thymic epithelial neoplasms? Interact Cardiovasc Thorac Surg. 2014 Jul;19(1):129-34. doi: 10.1093/icvts/ivu068. Epub 2014 Mar 19. PMID: 24648467.
5. Papatestas AE, Genkins G, Kornfeld P, Horowitz S, Kark AE. Transcervical thymectomy in myasthenia gravis. Surg Gynecol Obstet. 1975 Apr;140(4):535-40. PMID: 1129662.
6. Shrager JB, Deeb ME, Mick R, Brinster CJ, Childers HE, Marshall MB, Kucharczuk JC, Galetta SL, Bird SJ, Kaiser LR. Transcervical thymectomy for myasthenia gravis achieves results comparable to thymectomy by sternotomy. Ann Thorac Surg. 2002 Aug;74(2):320-6; discussion 326-7. doi: 10.1016/s0003-4975(02)03722-0. PMID: 12173807.
7. Meyer DM, Herbert MA, Sobhani NC, Tavakolian P, Duncan A, Bruns M, Korngut K, Williams J, Prince SL, Huber L, Wolfe GI, Mack MJ. Comparative clinical outcomes of thymectomy for myasthenia gravis performed by extended transsternal and minimally invasive approaches. Ann Thorac Surg. 2009 Feb;87(2):385-90; discussion 390-1. doi: 10.1016/j.athoracsur.2008.11.040. PMID: 19161744.
8. Friedant AJ, Handorf EA, Su S, Scott WJ. Minimally Invasive versus Open
Thymectomy for Thymic Malignancies: Systematic Review and Meta-Analysis. J Thorac Oncol. 2016 Jan;11(1):30-8. doi: 10.1016/j.jtho.2015.08.004. PMID: 26762737; PMCID: PMC7560956.
9. Abu-Akar F, Gonzalez-Rivas D, Yang C, Lin L, Wu L, Jiang L. Subxiphoid
Uniportal VATS for Thymic and Combined Mediastinal and Pulmonary Resections – A Two-Year Experience. Semin Thorac Cardiovasc Surg. 2019 Autumn;31(3):614-619. doi: 10.1053/j.semtcvs.2019.02.016. Epub 2019 Feb 21. PMID: 30796955.
info@onco-suisse
- Vol. 12
- Ausgabe 7
- Oktober 2022