- ISROI – Building a pathway for future-oriented radiation oncology
Radiation oncology (RO) is a medical discipline that utilizes various forms of ionizing radiation to treat malignant and benign diseases. RO is an essential clinical discipline; approximately 50-60% of cancer patients receive radiation therapy. RO, as a discipline, produces a considerable quantity of information and simultaneously consumes information created by other clinical fields. However, it is currently impossible to automatically exchange or utilize data created during routine clinical care. In this writing, we describe the evolution of the International Society for Radiation Oncology Informatics (ISROI) and its activities and provide examples of how the clinical workforce may contribute to developing a future-oriented informational landscape in radiation oncology.
Key Words: Radiation therapy, Information Science, Oncology, Data exchange, Semantic Interoperability
How radiation oncology and informatics are connected
Radiation oncology (RO) is a medical discipline that utilizes various forms of ionizing radiation to treat malignant and benign diseases. Radiation therapy (RT) is an essential part of treating patients diagnosed with cancer in curative or palliative settings. Approximately 50-60% of cancer patients receive radiation therapy as part of their treatment (1).
Information technology is an engineering domain that develops informational infrastructures, such as hardware, networks, applications, and performs their maintenance. Information science includes applied and academic disciplines involved in developing solutions and solving problems connected with information collection, processing, retrieval, computing, utilization, and many more aspects of information processing.
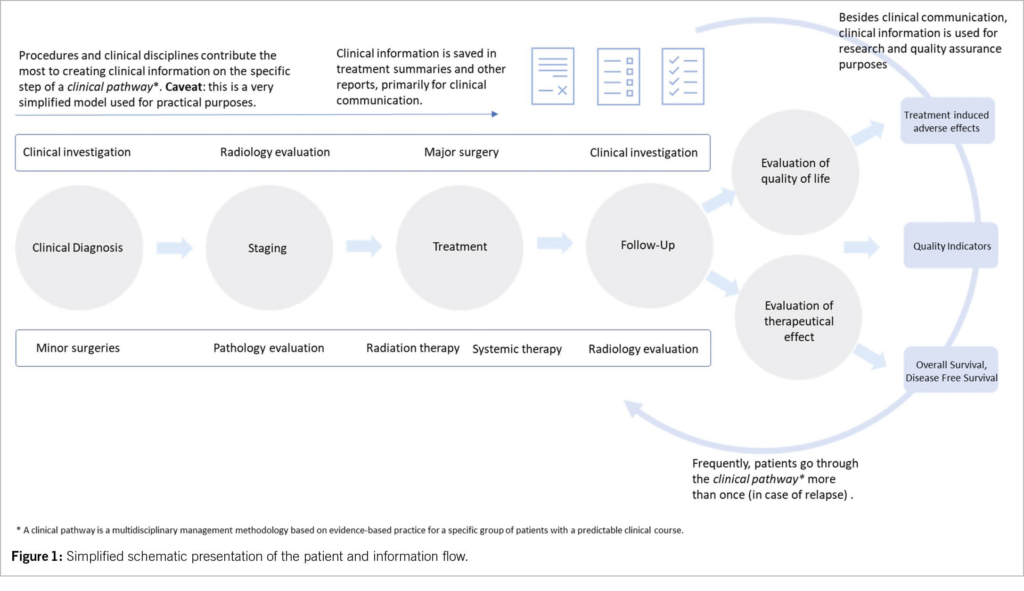
In RO, the previously mentioned domains are heavily interconnected and dependent on each other in the clinical setting. As a result, modern RT frequently requires complex hardware and software integration within RT departments and external partners. In addition, RT is data-intensive, where evermore information is created along the patient’s course of treatment (2). This course involves several steps. For example, before RT treatment starts, physicians evaluate the disease stage and choose the best diagnostic and treatment strategy. This requires multidisciplinary assessment and collaboration with other data-intensive disciplines such as radiology and pathology. Patients are usually discussed on interdisciplinary tumor boards, where the final treatment decisions are made. After that follows the preparation of the RT, which consists of many smaller substeps requiring interaction between patients and caregivers (e.g., consultation with RO specialists).
Furthermore, a planning computer tomography organization and consequent radiation therapy planning, as well as quality assurance procedures create additional data. In addition, treatment delivery and associated processes contribute to data heterogeneity. Finally, follow-up and regular checkups in interdisciplinary settings form an extra data layer. We present a short, simplified overview of the data and the patient pathway in Figure 1.
Such an environment provides a unique possibility to engage a variety of modern aspects of information science to develop and apply a foundation for precise and personalized RT care. Ideally, all data or derived information generated from multiple sources across the care continuum should be available at the right time to the right person (3, 4). Therefore, data and information should be integrated into one standardized, universally accepted electronic health record under the patient’s direct control.
However, achieving such a level of integration is very difficult. For example, it has been shown, that fewer than one in three hospitals can find, send or integrate health-related information from another provider (5, 6). More recent studies additionally reveal significant problems in data management. For instance, inter-vendor data exchange on very minimal and highly standardized datasets, namely laboratory values and medications, is below 15% (7). Despite some progress in data interoperability, the problem is unlikely to be solved anytime soon. Furthermore, poorly designed user interfaces combined with inadequate workflows and user experience result in severe consequences. For example, recent study on clinical information systems and electronic health record in Switzerland showed that is almost impossible to make all medication prescriptions correctly (8, 9). Therefore, a new way of collaboration at all levels of healthcare is needed.
What does this mean?
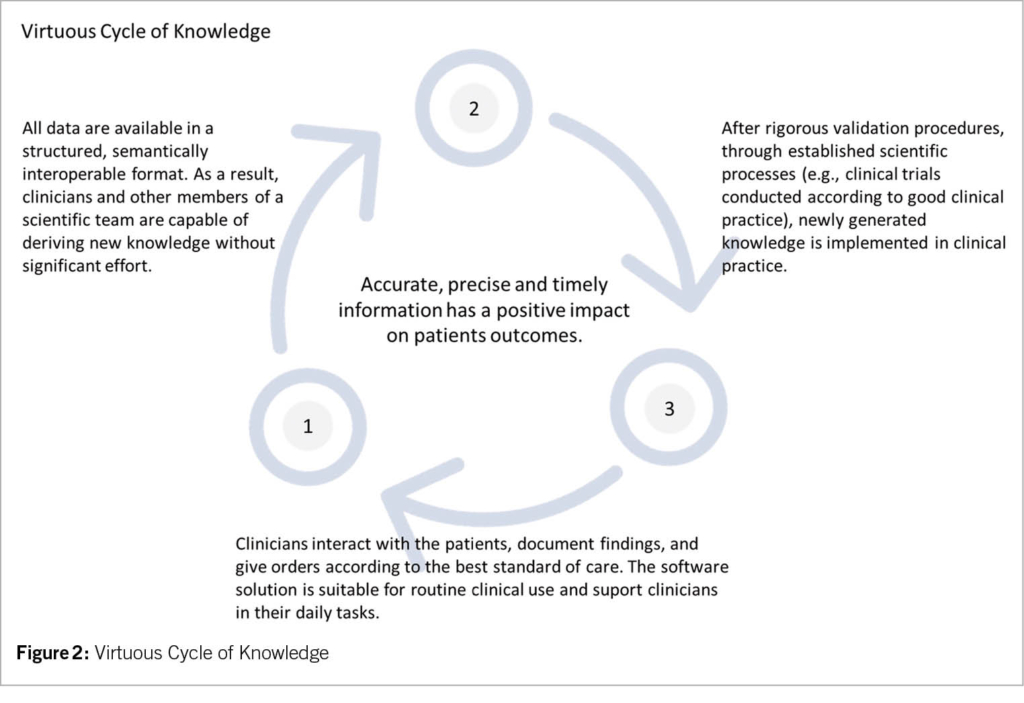
Precise, personalized, and affordable healthcare will only be possible if the information is shared between all interested parties without technical or other obstacles. Furthermore, physicians, physicists, nurses, and radiation therapists must have a working environment that efficiently and effectively facilitates data-intensive tasks. Therefore, we need an additional communication layer on a syntactic and semantic level. On a practical level, we must be capable of transforming domain knowledge, which exclusively lies within the clinical environment and professional societies into computable and sharable formats. We must convert domain knowledge into the condensed form of computable clinical guidelines and common reusable data elements (4). Such transformation will create a virtuous cycle of knowledge (Figure 2).
The clinical information technology environment must adapt to everchanging requirements, implement new methodologies and new models, and fulfill the needs of healthcare workers and patients. In addition, patients should be empowered to control all of their data and share it between institutions, without significant effort, for clinical or research purposes. Finally, all data created during a disease course must be findable, accessible, interoperable, and reusable (10, 11).
What challenges do we have to confront?
Such a massive undertaking is not possible without fundamental changes and effort across the biomedical enterprise. The clinical environment is complex and interconnected with all aspects of society and dependent on sociological, political, and economic factors. Any systemic change requires interventions and movements across all levels.
The role of radiation oncology
RO is an already highly «digitalized» clinical domain. In modern RO, informational infrastructure is basic. It is an interconnected clinical discipline that consumes and produces large amounts of information and data. In order to treat a patient according to the latest standards of care, images created in radiology departments are used, pathology reports are evaluated while coordination with medical oncology and other disciplines for combined systemic treatment is crucial. With this in mind, we have founded ISROI as a society that aims to translate and transform theoretical and practical knowledge into a form suitable for a clinical environment.
ISROI history and role
ISROI has evolved from annual Radiation Oncology Informatics (ROI) meetings held in St. Gallen (CH) and Freiburg (D). ROI meetings were a platform for exchanging the latest developments in practical and research domains in clinical and administrative informatics tightly connected with RO. Through the years, contents of increasing quality and quantity were presented. As a result, the number of presenters and attendees grew. For this reason, members of a board decided to transform ROI meetings into a more suitable format. On 12.05.2020, in St. Gallen, board members officially agreed on the articles of association and formally founded ISROI. ISROI includes members from all domains of radiation oncology and connected disciplines. Currently, ISROI has 53 members from five countries.
The primary goal of the ISROI is to improve patient care and outcomes by advancing informatics in RO.
This higher goal is, however, achievable only by fulfilling subordinate goals. Therefore, we concentrate on our development milestones as follows. On the academic level, we have three major goals. First, ISROI will establish radiation oncology informatics as an academic discipline. Besides pure engineering principles, we want to introduce scientific methodology into the field. Second, we aim to educate the next generation of professionals. With our activities, we would support development through all stages of education. Third, we will promote and distribute knowledge created through our activities by disseminating scientific publications, organization of scientific meetings, and guest lectures. In the long term, we will support developing and maintaining a radiation therapy curriculum.
Further goals are practice-oriented. ISROI members will promote value-based radiation oncology and implement best clinical practices as a primary goal for the clinical environment. Furthermore, ISROI will actively contribute to optimizing clinical workflow and promote meaningful digitalization in RO and other clinical disciplines. We believe that improving the digital work environment will result in direct, measurable benefits for the clinical workforce. More ergonomic digital solutions should improve process quality, worker’s satisfaction and data quality, ultimately elevating safety and improving patient outcomes. Lastly, ISROI understands the importance of technical and semantic interoperability of data within and beyond the RO domain. Besides common practice and accompanying challenges in the clinical routine, we are witnessing the remarkable development of new artificial intelligence (AI) approaches. These technological advancements impose additional challenges for clinical departments. Development, implementation, validation, and verification of AI-based solutions will result in new challenges and requirements for a workforce equipped with new skills. ISROI will dedicate significant effort to early recognition of such needs and guiding for appropriate solutions. Therefore, we are engaged in developing semantic and syntactic resources for clinical routine and research purposes.
The next level of ISROI activities is concentrated on the administrative and managerial aspects. With our efforts in establishing the informational infrastructure standards, we will contribute to better transparency, efficient workflows, and proper billing. In addition, we would like to develop a new quantifiable measurement system such as key performance indicators for RO departments. This would allow hospitals to have a better foundation for its decisions.
ISROI activities are not exclusively oriented to the clinical environment. Essential aspects of our efforts are oriented toward developing new models for collaboration with the industry. We act as a facilitator of the communication process between users and manufacturers of RT equipment and software.
By incorporating all the activities mentioned above, ISROI will contribute to developing policies and regulations in the domain of radiation therapy.
Conclusion
The International Society for Radiation Oncology Informatics – ISROI is an excellent example of how the clinical workforce may contribute to developing a future-oriented informational landscape in radiation oncology. In addition, ISROI may serve as a model for other clinical domains.
Nikola Cihoric 1,5, Fabio Dennstädt 2,5, Heuser Michael 3,5,
Peters Samuels 2,5, Meinschad Marco 4,5, Paul Martin Putora 2,5
1 Department of Radiation Oncology, Inselspital, Bern University Hospital, University of Bern, Bern, Switzerland.
2 Department of Radiation Oncology, Kantonsspital St. Gallen, St. Gallen, Switzerland
3 Department of Radiation Oncology, Kantonspital Aarau
4 Academic Teaching Hospital, Institute of Medical Physics, Feldkirch, Austria
5 International Society for Radiation Oncology Informatic – ISROI
Copyright bei Aerzteverlag medinfo AG
Department of Radiation Oncology, Inselspital,
Bern University Hospital, University of Bern, Bern, Switzerland.
International Society for Radiation Oncology Informatic – ISROI
Dr. Nikola Cihoric is a technical lead for SmartOncology© project and medical advisor for Wemedoo AG, Steinhausen AG, Switzerland
1. Delaney G, Jacob S, Featherstone C, Barton M: The role of radiotherapy in cancer
treatment: estimating optimal utilization from a review of evidence-based clinical guidelines. Cancer 2005, 104(6):1129-1137.
2. Putora PM, Peters S, Bovet M: Informatics in Radiation Oncology. In: Machine Learning in Radiation Oncology: Theory and Applications. edn. Edited by El Naqa I, Li R, Murphy MJ. Cham: Springer International Publishing; 2015: 57-70.
3. Pronovost PJ: Procuring interoperability: achieving high-quality, connected, and person-centered care: nam. edu; 2018.
4. Osterman TJ, Terry M, Miller RS: Improving Cancer Data Interoperability: The Promise of the Minimal Common Oncology Data Elements (mCODE) Initiative. JCO Clin Cancer Inform 2020, 4:993-1001.
5. Turbow S, Hollberg JR, Ali MK: Electronic Health Record Interoperability: How Did We Get Here and How Do We Move Forward? JAMA Health Forum 2021, 2(3):e210253-e210253.
6. Holmgren AJ, Patel V, Adler-Milstein J: Progress In Interoperability: Measuring US Hospitals’ Engagement In Sharing Patient Data. Health Aff (Millwood) 2017, 36(10):1820-1827.
7. Bernstam EV, Warner JL, Krauss JC, Ambinder E, Rubinstein WS, Komatsoulis G, Miller RS, Chen JL: Quantitating and assessing interoperability between electronic
health records. J Am Med Inform Assoc 2022.
8. Wright AA, Katz IT: Beyond Burnout – Redesigning Care to Restore Meaning and Sanity for Physicians. N Engl J Med 2018, 378(4):309-311.
9. Fischera S, Schwappachb DLB, Sojere R, Kraftg E: Effizienz und Patientensicherheit von Klinikinformationssystemen. Schweizerische Ärztezeitung 2021, 102(46):1516-1520.
10. Wilkinson MD, Dumontier M, Aalbersberg IJ, Appleton G, Axton M, Baak A, Blomberg N, Boiten JW, da Silva Santos LB, Bourne PE et al: The FAIR Guiding
Principles for scientific data management and stewardship. Sci Data 2016, 3:160018.
11. Wilkinson MD, Dumontier M, Jan Aalbersberg I, Appleton G, Axton M, Baak A, Blomberg N, Boiten JW, da Silva Santos LB, Bourne PE et al: Addendum: The FAIR Guiding Principles for scientific data management and stewardship. Sci Data 2019, 6(1):6.
info@onco-suisse
- Vol. 13
- Ausgabe 1
- Februar 2023